

TeamSTEPPSIPE Research Module


Simulation Using TeamSTEPPS To Promote Interprofessional Education & Collaborative Practice
Loyola University Chicago - Health Science Division
Institute for Translational Interprofessional Education
This learning module provides a focused introduction to TeamSTEPPS as a performance improvement process.
It will serve as the educational content for a research study looking at the impact of simulation using TeamSTEPPS
principles to promote Interprofessional Education and enhance team-based patient care.
TeamSTEPPS
The Four Pillars
The TeamSTEPPS system believes that effective teams
are built upon the foundation of four essential pillars or
cornerstones:
This module will provide you with an understanding of these team dynamics.
To begin let's take a moment to lay out the goals and objectives for this learning experience.

GOALS AND OBJECTIVES
This interprofessional learning module which focuses on TeamSTEPPS is meant to enhance team performance in a simulated
patient care environment.
Upon completion of this module the learner will demonstrate:
PRINCIPLES, STRATEGIES AND TOOLS
This module will introduce and discuss TeamSTEPPS strategies for effective communication and enhanced team functioning.
The learner should understand and be prepared to demonstrate the following TeamSTEPPS elements and related tools:
In order to demonstrate the proper application of TeamSTEPPS, participants will participate in an interprofessional patient-care simulation.
The focus of this exercise will be on utilizing TeamSTEPPS strategies.
Interprofessional teams participating in this cohort study will be assessed on their performance according to TeamSTEPPS principles.
As you study this module, you should do so with an eye toward how the behaviors described would be carried out in your clinical setting.
This will help you to begin to translate theoretical knowledge into a practical application of the desired team skills.
Throughout the module, you will receive practical tips and strategies for incorporating TeamSTEPPS behaviors.
Please advance to the next page to begin this TeamSTEPPS learning module.
Why We Must Be Concerned
A report published by the Institute of Medicine revealed that:
Estimates suggest that the cost associated with medical errors is $8–29 billion annually.
In response to this data the Federal Government called for action...
By 5 years;
TO ACCOMPLISH THIS GOAL WE CAN'T OVERLOOK THE FACT THAT:
Root-cause-analysis studies reveal that medical errors are often related to system errors -
breakdowns in the expected performance of groups or teams.

TeamSTEPPS
Team Strategies and Tools for Enhanced Performance and Patient Safety
Background and Context
Who doesn't want to ensure patient safety?
Who doesn't want to be better as a clinical care provider?
What group, organization or team doesn't believe that they can be more effective or successful at what they do?
How, then, do we overcome the inertia and the obstacles to make our goal a reality?
Read on to discover how...
Be All You Can Be!
This slogan, coined by the U.S. Army, speaks to the drive in each of us to fulfill our potential.
Many individuals muddle along without achieving their full capacity, yet some go farther,
rise higher, and succeed in achieving their goals.


TEAMS, GROUPS, ORGANIZATIONS
This is also true for groups. If individuals struggle to achieve their capacity,
how much more do groups operate less effectively than is essential for safe patient care.
Click here to see what we mean!
[Click on the play button, then click again on the screen to enlarge the picture]

PATIENT CENTERED TEAM CARE
What's At Stake?
Contemporary health care is an increasingly interprofessional, team-based process
where the health and well-being, if not the very life of a patient, is the priority and focus.
With such high stakes, there is no room or excuse for muddling along.



Barriers to Effective Team Performance
If team (under)performance is a critical part of the problem, then how must we respond?
What keeps us muddling along?
What are the barriers that must be overcome for a team to perform at desired levels?
Experience has shown that the great barrier to effective team performance is
innefective communication.
Additional hurdles that must be overcome include:
We Can Solve This
If the underperformance of teams is at the root of the problem,
then strengthening teamwork must be our solution.
TeamSTEPPS was created to provide a mechanism for developing effective teams.

Establishing a Team
Teamwork cannot begin, or be successfully achieved, unless a team is properly identified and established.
The process begins as a group of individuals is identified and established as a Core Team.
Teams are typically constituted by formal, institutional, or organizational processes in response to needs.
But teams can also emerge in situations where circumstances call for the prompt, effective and coordinated actions of a cohesive group (team) whose
members have unique, but interdependent skill sets.
For purposes of this learning exercise, you should be mindful of the need to promptly identify and make clear who are members
of the team, and who is the designated or assigned leader of the team.
Demonstrating that a team has been properly established is the important first step in this process.
EXAMPLE:
Team Member 1: (Carol, RN) "We have an acutely ill asthmatic patient with shortness of breath. To handle this case we will need a nurse,
physician and respiratory therapist to be involved in the patient's initial management."
Team Member 2: (Edward, RT) "Dr. Jones will you take leadership as we stabilize the patient and determine the exact cause of her respiratory distress?"
Team Member 3: (Paul, MD) "That's fine with me. I will need you, Carol, to get the patient on a monitor, obtain a set of vital signs including an O2 saturation,
and ensure that the IV that was started in the ambulance is still functioning properly. Please inform me of the oxygen saturation and we will institute oxygen therapy.
Team Member 1: (Carol) "I will put her on a monitor, check her O2 sat, place her on 2 liters nasal oxygen if needed, and check the status of her IV.
Do you also want me to obtain a 12-lead EKG?"
Team Member 3: (Dr. Jones) Absolutely, and can you also call Radiology for a portable Chest XRay?" Ed, can you give the patient a neb treatment and draw a blood gas for us?
Team Member 2: (Edward, RT) "I will start her neb treatment, and then draw an ABG."
Getting the Most from Your Team
Recognizing that some of the most important work we do each day is done
within the structure of some form of team, we need to understand what
teams are and what helps to make them effective.
What is a Team?
Two or more people who interact dynamically, interdependently, and adaptively
toward a common, shared and valued goal, have specific roles or functions, and have a
time-limited membership.
Why a team?
Teamwork cannot occur in the absence of a clearly defined and committed team.
Improving upon an existing, or designing a new team structure, is the first step
in implementing an effective teamwork system in any environment.
Effective TEAM MEMBERS:
To See What an Effective Team Looks Like
[Click on the play button, then click again on the screen to enlarge the video]
KEY POINTS:
In this video you should have recognized aTEAM LEADER who:
"The ratio of We's to I's is the best indicator of the development of an (effective) team."
-Lewis Ergen

Building an Effective Team
TEAMS that perform well:
(Salas et al. 2004)
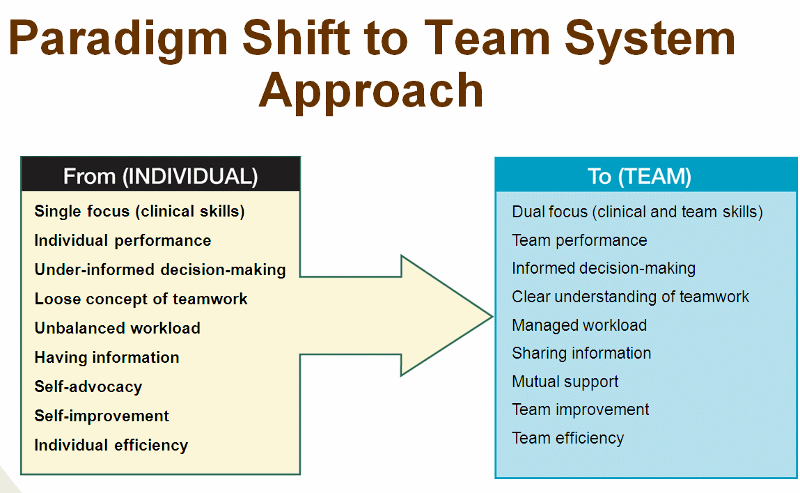
Building effective teams requires a paradigm shift in thinking and emphasis..
It requires a substantive change in thinking and acting, moving from a focus
on individual goals and performance to team goals and interdependent behaviors.

TeamSTEPPS
The Four Pillars
As we said at the beginning of this module the TeamSTEPPS system believes that effective teams
are built upon the foundation of four essential pillars or cornerstones:
We shall now carefully explore each of these four areas.

Leadership
Leadership is the lynchpin that holds a highly effective team together.
It is the ability to coordinate the activities of team members and teams by
managing the resources available to team members and facilitating team
performance by communicating plans, providing and updating information
about team performance through debriefs, and providing support to team
members when needed.
In a new era of health care and patient management, interdisciplinary
co-management is increasingly being emphasized.
However, quality interdisciplinary co-management still requires the
designation of a leader to effectively guide the team and manage team
resources.
[For purposes of this TeamSTEPPS training, you should be aware that
any team that operates without an assigned leader is a suboptimal team!]
There are two types of leaders:
This is an important concept for it reminds us that in certain situations any member of the team
may be expected to exercise leadership within their area of competence.
Effective leadership is critical to the success of any team.
But none of the processes below can be done effectively or accountably unless
the team is clear about who the leader is.
Effective leaders:
Effective leaders cultivate desired team behaviors and skills through:
The last item in this list is so important the we will take a moment to look at each of the three activities.

Team Events
Leaders are responsible for assembling the team and facilitating team events.
Three useful activities that are designed to promote team effectiveness are:
Anyone can request a team activity if the sitiuation calls for it!
[Recall what was said earlier about designated vs situational leadership]
Let's now take a moment to make sure we know what each of these activities are
so that you can use them effectively within your team(s).
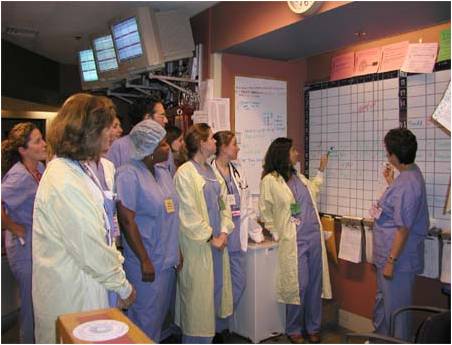
Briefs
Briefs are short gatherings of team members, prior to the start of a shift, or an event, or activity that focuses on
anticipation and planning.
These sessions, as their name suggests, are meant to be brief, concise and empowering.
They serve to:
Use of a check-list can help to maximize efficiency during a brief.
Effective teams organize themselves in anticipation of the activities and events they will face.

Huddles
Huddles are ad hoc, touch-base moments meant to re-establish situation awareness,
reinforce plans already in place, or assess the need to adjust pre-determined plans.
Huddles are designed to effect Problem Solving at any point in the work-day.
They are used to:

De-Briefs
De-Briefs are about process improvement.
Debriefs:
As with Briefs, De-Briefs can be optimized by using an appropriate De-Brief Check-List.

Effective teams commit themselves to taking the time at the conclusion of a shift or event to
look back critically at the team's performance and identify corrective actions for going forward.
If teams ignore the process of debriefing, then suboptimal behaviors are given tacit approval,
and performance improvement is limited or hindered.
For purposes of this TeamSTEPPS training, the expectation will be that at the end of any
patient management activity, the team should conclude the activity with the team leader taking
a moment to "de-brief" the team on their performance with respect to communication,
situation awareness, and mutual support, as well as seeking any feedback on the leadership
that was exercised.
Leadership
We have just looked at how good leaders can use tools like Briefs, Huddles, and De-Briefs
to overcome barriers to team performance and promote desired outcomes.
We shall now turn to the second pillar of effective team performance - Communication.

Communication
Communication is the process by which information is clearly and accurately exchanged
among team members.
No team can succeed without effective communication. It is the critical lifeline.
Conversely, communication breakdowns are a contributing factor to team underperformance.
Ineffective communication is the root cause of a significant percent of sentinel events (medical errors)
reported in clinical settings.
How, then, can we ignore this?
Experience has shown that there are multiple barriers to effective communication:
Standards of Effective Communication
For communication to be effective it must be clear, complete and concise:
Let's take time now to look at some techniques that can insure that our
communication is effective.

Enhancing Communication
There are several techniques or tools that can help to strengthen team communication:
SBAR is a framework for team members to structure information exchanges when communicating
with one another.
It is meant to help make information clear, complete and concise.
When communicating using SBAR you should:
State the Situation of concern immediately and concisely so your listener understands the point of concern.
You should then place your concern in the context of relevant Background information.
You should then provide your listener with your Assessment of the situation, followed by your
Recommendation of what you believe needs to be done to address the situtation.
[For an example of SBAR, click the play button, then double click on the screen to enlarge the video]
Some other examples of SBAR communication that you can use to shape your communication skills:
Nurse (speaking on phone to physician):
S: I'm calling you about a patient, Mrs. S.B. whose mental status seems to have changed..
B: She's 75 years old and had a hip fracture repaired yesterday.She did well for the first 24 hours
but this evening she seems confused and a bit restless in bed. Her temperature is slightly elevated
at 99.5 degrees, her blood pressure is 114/69, her HR is 96 and her 02 sat is 90%.
Her incision does not reveal signs of infection, and other than her confusion her physical exam and
her neurological status is unchanged. She's been on Norco for the past 24 hours as her only new medication.
A:This might just be from the Norco she's receiving, or perhaps she could just be "sundowning," but I don't think
we can exclude early sepsis, or even a pulmonary embolism as the cause.
R:I'm concerned and would like you to come and assess her to make certain we don't ignore anything that could be serious.
ED Physician (speaking to respiratory therapist)
S:I need for you to help me with a dyspneic patient here in the Emergency Department.
B:The patient is a 74 y/o male with known COPD, and multiple hospitalizations for shortness of breath.
His 02 sat is 84% and his PCO2 is 52.
The last time he was in the hospital he required intubation for a prolonged period of time.
He now states that he no longer wishes to be intubated (DNI) as part of his treatment.
A: He has a right lower lobe pneumonia for which he has agreed to inpatient treatment with IV antibiotics
R: I need for you to come and set him up on BIPAP.
"The patient's blood pressure is dropping!"
"I am having difficulty getting a peripheral IV."
"I don't like the way the patient looks!"
"I'm seeing an increase in fetal decelerations!"
Effective team members feel empowered to call out whenever the need arises, recognizing that the ultimate goal
is the safety of the patient and the success of the team.
[For an example of a Call Out, click the play button, then double click on the screen to enlarge the video]
The sender initiates the message, the receiver accepts it and restates the message,
in return, the sender verifies that the re-statement of the original message is correct or
if not, amends it.
Leader: "Nurse Jones: I wan't you to administer one amp of 50% Dextrose IV.
Nurse Jones: "I am ready to give one amp of 50% Dextrose IV."
Leader: "Dr. Richards, when the patient is adequately sedated I want you to charge the defibrillator
and perform a synchronous cardioversion at a setting of 100 Joules."
Dr. Richards: "I will prepare the defibrillator to perform synchronized cardioversion at a setting of 100 Joules."
[For an example of a Check Back click the play button, then double click on the screen to enlarge the video]
[Click the play button, then double click on the screen to enlarge the video]
Having explored strategies for enhancing communication, let us now turn to the third pillar of effective
team performance, Situation Monitoring.

Situation Monitoring
"Attention to details is one of the most important details."
Situation Monitoring:
Is the process of continually scanning and assessing what's going on around you to maintain situation awareness.
It is made possible by a state of vigilant mindfulness related to team functioning with respect to a desired or pre-determined outcome.
In simple terms it is the state of "knowing the current conditions affecting a team's work."
It is a process of actively scanning behaviors and actions to assess elements of the situation or environment
With a shared mental model, it helps to assure that all team members are "on the same page."
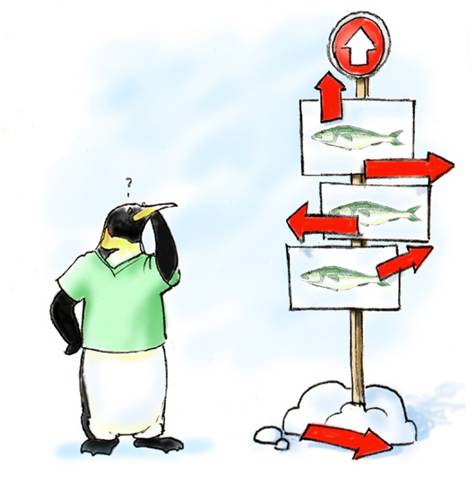
To begin our discussion of Situation Monitoring, let's look at a humorous example of poor Situation Monitoring.
[Click the play button, then double click on the screen to enlarge the video]
The foundation or starting point of effective situation monitoring is achieving a shared mental model.
We will now look at what this means.
SHARED MENTAL MODEL
This means "everyone being on the same page."
It is a mental picture or sketch of the relevant facts and relationships defining an event,
situation or problem.
Shared mental models are knowledge structures of the relevant facts and relationships
about tasks or situations that the team is engaged in, and about the way the team members
interact. Shared mental models enable the team to anticipate and predict each other's needs.
A good team must track whether team performance is moving in the right direction, at
the right pace, with the necessary efficiency.
"Teams that perform well hold shared mental models." (Rouse, Cannon-Bowers, and Salas 1992)
Here is an example of what happens when a team doesn't have a shared mental model and its members
fail to communicate effectively.
(Click the play button, then double click on the screen to enlarge the video)
Shared Mental Models:
" Shared mental models help teams avoid errors that place patients at risk."
Example:
Team Leader: "Our goal is to get the epidural anesthetic administered quickly and safely, proceed with the C-Section with
the goal of getting the baby delivered as quickly as possible, while simultaneously monitoring the mother for any adverse
reactions to the anesthesia during the procedure.
Is everyone clear about their responsbilities?"
Having explained the importance of a shared mental model, let's return now to complete our discussion of Situation Monitoring.

SITUATION MONITORING:
Let's look at two tools designed to structure the process of Siituation Monitoring.
1. Cross Monitoring
Cross monitoring is an error reduction strategy that involves:
The scenario below illustrates the dynamic of situational awareness and cross monitoring:
Scenario:
A patient in the ICU has coded, and CPR is in progress. The Resuscitation Team is busy
ensuring that intravenous access is available, and the ET tube is inserted correctly.
Dr. Matthews, the Team Leader, is calling out orders for drugs, X-rays, and labs. Judy, a
nurse at the bedside, is inserting an IV. Nancy, another nurse, is drawing up meds. Judy
can tell by Nancy's expression that she didn't get the last order called out by Dr. Matthews.
Judy calls out while continuing to place the IV, "Nancy, he wants the high-dose epinephrine
from the vial in the top drawer."
2. S.T. E.P.
S.T.E.P. is a mnnemonic that helps us to organize our mindfulness and allows us to acquire a trained eye
for monitoring elements that are critical to the situation.
The elements that make up S.T.E.P. are:
The following example illustrates each component in the STEP process.
Example:
The repiratory therapist notes that an intubated patient is showing a
marked increase in respiratory rate that might indicate increased pain
that the patient cannot communicate. (STATUS OF PATIENT)
The patient's nurse is busy helping another patient. (TEAM MEMBERS)
It is shift change, and everyone is busy, so you check the medication record
and note that the patient is overdue for his morphine. (ENVIRONMENT)
You notify the oncoming nurse of your concern and make a recommendation. (PROGRESS)
Let's conclude by looking at the final pillar upon which effective teams are built - Mutual Support.

Mutual Support
"A chain is only as strong as its weakest link."
Mutual Support is the essence of teamwork.
It protects team members from work overload, and helps them in conflict situations
that may reduce effectiveness and increase the risk of error.
There are four helpful tools that can foster the process of mutual support.
They are:
1. Task Assistance: Team members foster a climate in which it is expected that assistance
will be actively sought and offered as a method for balancing workloads and reducing the
occurrence of error.
2. Feedback: Feedback is the giving, seeking, and receiving of performance-related
information among the members of a team for the purpose of improving team performance.
It is the ability to communicate self-improvement information to others in a useful way.
3. Advocacy and Assertion: Two techniques for intervening when your viewpoint does not
match that of the decision maker.
In advocating for the patient and asserting a corrective action, the team member has an opportunity
and a responsibility to correct errors or reinstate situational awareness.
Failure to employ advocacy and assertion has been identified as a primary contributor to
clinical errors.
The goal is to assert a corrective alternative in a firm, but respectful manner.
When viewpoints are in conflict, always act as an advocate for the patient.
Example:
The following is an example of this process:
4. Conflict Resolution:
There are two types of conflict that teams face -
Let's take a moment to learn more about some tools for resolving these two forms of team conflict.



Conflict Resolution
All teams must exercise strategies for resolving informational or interpersonal conflict if they are to be truly effective and mutually supportive.
There are three tools for conflict resolution:
When dealing with conflicting information, or conflicting views of a problem:
1. Two Challenge Rule: Invoked when you believe information is incorrect or an assertion
is ignored or resisted…
An Example:
Leader: "I'd like you to give the patient Morphine 40 milligrams IVP."
Team Member: "That seems to me to be too large a dose." (Challenge One)
Leader: : "I always give 40 mg to start when a patient is in congestive heart failure!"
Team Member: "I think you may be confusing medications." (Challenge Two)
"Do you mean 40 milligrams of Morphine or 40 milligrams of Lasix?"
Leader: "Thank you for catching that error, I meant to say 40 milligrams of Lasix, and 4 mg of Morphine."
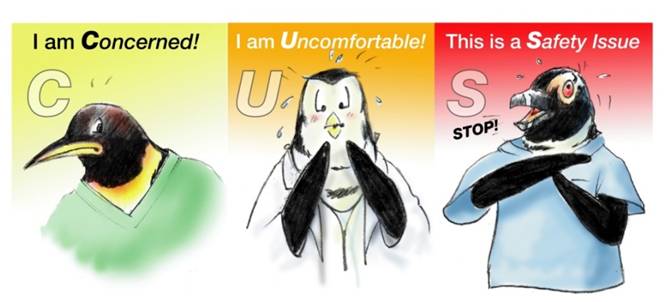
2. Use of the CUS words: Concerned, Uncomfortable, Safety
This technique for conflict resolution uses signal phrases that denote:
An Example:
Team Member #1: "I am concerned that is taking too long to get the endotracheal tube in place."
Team Member #2: "We've tried several times, and we're going to try again."
Team Member #1: "I am uncomfortable that it has already been several minutes."
Team Member #2: "I've never missed getting an airway, and this case should be no different."
Team Member #1 "I don't believe it is safe to keep trying, I am calling for anesthesia right now!"
When this technique is properly employed, all team members should understand clearly not only
the issue, but the magnitude of the issue.
Occasionally team conflict stems, not from disputes over information or strategies, but over
team members' behaviors.
When dealing with interpersonal conflict within a team, a structured approach that addresses
the conflict while remaining respectful of conflicting team members is warranted.
The technique for resolving behavior conflict is called "DESC" Script and the steps in the process are listed below.
3. DESC Script: A constructive mnemonic appproach to resolving interpersonal conflict among team members
D—Describe the specific situation (state the facts accurately)
E—Express your concerns/feelings about the action or behavior
S—Suggest a constructive alternative
C—Consequences are stated for failure to respond professionally
NOTE:
As a general rule DESC-ing is best done by taking time to collect and write out one's thoughts about
the conflict, and then addressing them with the individual after a brief "cooling off" period. If necessary
one may wish to bring a third team member along as an observer, or referee. The goal should be win-win
for each party and allow for securing team unity despite conflicts.
An Example:
Team Member #1: Can we talk for a moment about yesterday?
Team Member #2: Sure what do you wish to discuss?
TM #1: Yesterday you came into a patient's room where I was working, and expressed your displeasure
that orders you had left on another patient were not yet carried out. Your tone presumed that I had
ignored your orders, or that I was not doing my job satisfactorily. What you weren't aware of was that
the patient I was working with was a critically ill patient and a higher priority at the time.
TM #2: I didn't know that you were dealing with a higher priority when I was talking to you.
TM #1: You never asked before launching into your criticism, and criticizing me in front of my patient
undermined my credibilty.
TM #2: I was concerned and upset that my patient hadn't gotten the care I had ordered.
TM #1: I can appreciate your being upset, but handling it the way you did was not very professional.
I would ask in the future that when you have a concern, you share it in private with me, so that we can
get to the facts and resolve it professionally.
TM #2: You're right, I acted unknowingly and didn't consider the consequences. Thank you for pointing
this out. I will try to not let it to happen again.
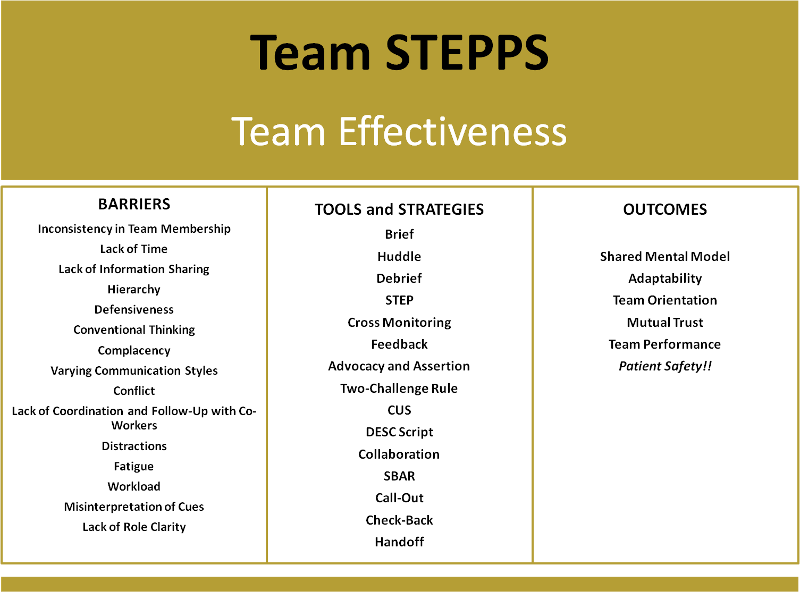
Conclusion
We began this journey with the belief that there is always room for improvement, and when it comes to team effectiveness
you need good strategies to overcome barriers and tools to achieve your goal.
The final slide below summarizes the challenges, the tools and the related outcomes that are possible when employing a
Team STEPPS approach in any organization.
We hope that you will make it a policy and priority to employ these tools effectively in whatever team you find yourself working with.
FINAL RECOMMENDATIONS
In the performance assessments that will be a part of this research study of team behaviors, you will be assessed on your ability to demonstrate
the team behaviors you have learned in this educational module.
Specifically, you should be very intentional about the need to:
1. Establish/identify your team (members), designate a team leader and maintain leadership throughout the event.
2. The leader should brief the team in a way that creates a shared mental model or plan for what is to be undertaken.
3. Clearly define and delegate roles and responsbilities, holding members responsible and accountable.
4. Seek from and communicate necessary infomation to members in brief, timely, clear, concise fashion.(SBAR)
5. Verify all information that is communicated, especially when part of an order. (Check Back)
6. Cross monitor the performance of team members to assure that you are progressing toward your goal.
7. Provide mutual support to one another in order to maximize your resources.
8. Advocate boldly and assert yourself respectfully but definitively for the patient whenever issues of patient safety are at stake.
9. Use effective strategies to resolve conflict - Two Challenge Rule, and CUS (concern, uncomfortable, safety)
10. Collaborate constructively with fellow team members, by de-briefing after every event in order to provide constructive feedback.
Please Proceed to the Next Page and Complete the Self Assessment Quiz.

Test Your Knowledge
Use the following questions to assess your grasp of the concepts, principles and processes related to TeamSTEPPS.
You Have Completed This Learning Module.